Many people rely on familiar medications to ease pain, soothe heartburn, help with sleep, or manage everyday discomforts. These treatments can be helpful when used occasionally, yet long-term use can introduce concerns that healthcare professionals watch closely. Over time, daily or frequent use of certain drugs may influence the kidneys, digestive system, or bones, according to research often referenced by organizations such as the American Geriatrics Society.
If you take any of these medications regularly, it is useful to understand why doctors evaluate their benefits carefully while keeping an eye on possible long-term effects. The positive news is that safer approaches and more mindful routines can often support your health while reducing unnecessary risks. You will also find practical ideas you can bring to your healthcare provider, and near the end, you’ll see how simple lifestyle adjustments may help you depend on fewer medications over time.
Why Long-Term Medication Use Raises Questions
Doctors continue to prescribe these medications when needed, since they are effective when used appropriately. Still, clinical guidelines such as the Beers Criteria highlight the importance of caution, especially for older adults or individuals with specific medical conditions. Extended use may raise the chances of organ strain or medication dependence. Awareness is the key: understanding these possibilities helps you communicate clearly and confidently with your healthcare provider.
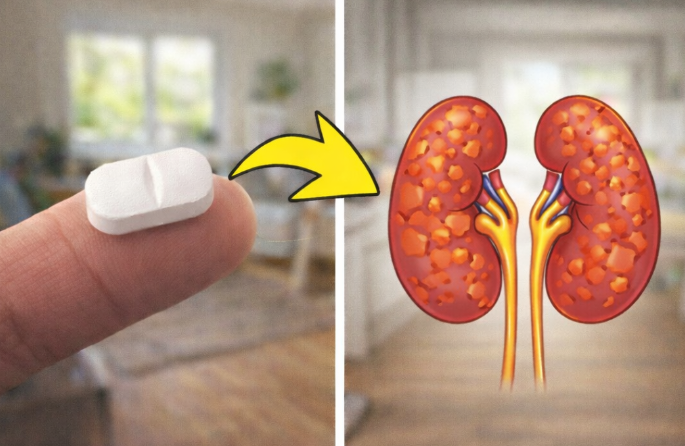
1. Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) – such as Ibuprofen and Naproxen
NSAIDs are commonly used for headaches, joint discomfort, and muscle soreness. They are widely available and work by reducing inflammation.
Long-term use, however, has been linked to concerns involving kidney function, elevated blood pressure, and irritation of the stomach lining. Groups like the American Geriatrics Society advise limiting frequent long-term use when alternatives can be considered.
Kidney stress can increase gradually, especially when higher doses are taken routinely or when a person already has risk factors.
A simple way to stay mindful is to track how often you use them. Many people find that rest, light stretching, or warm compresses reduce their need for NSAIDs. Some switch to occasional acetaminophen instead, which can be gentler for many individuals when used responsibly.
2. Proton Pump Inhibitors (PPIs) – such as Omeprazole and Esomeprazole
PPIs help manage acid reflux, heartburn, and ulcer prevention. They are effective, yet extended use has been connected in studies to changes in nutrient absorption, specifically calcium, magnesium, and vitamin B12. These factors may influence bone health or kidney function if monitored incorrectly.
Doctors often reassess whether long-term use is still necessary. Lifestyle changes can provide meaningful improvement, such as eating smaller meals, avoiding trigger foods later in the evening, and sleeping with the upper body slightly elevated. Many individuals benefit from taking short breaks from PPIs under medical supervision.
3. Acetaminophen (Paracetamol) – such as Tylenol
Acetaminophen is typically considered a simpler option for pain or fever because it does not irritate the stomach the way NSAIDs can. Even so, exceeding recommended doses over long periods may affect the liver. Since acetaminophen is included in many multi-symptom cold medicines, accidental overuse is common.
To stay safe, it helps to check every label, limit daily amounts to recommended guidelines, and avoid alcohol if you take acetaminophen frequently.
4. Benzodiazepines and Certain Prescription Sleep Aids
These medications help with anxiety or sleep concerns and can work quickly. Long-term use, though, may lead to dependency, a need for higher doses, or possible impacts on memory and balance.
Many people successfully transition to non-medication strategies. A consistent bedtime routine, reduced screen time in the evening, and cognitive behavioral tools for insomnia frequently lead to better long-term results. If someone is already using these medications, a doctor can guide them through a gentle tapering process.
5. Certain Antihistamines – including Diphenhydramine
Many over-the-counter sleep aids or allergy products rely on older antihistamines, which can cause drowsiness, confusion, or dry mouth, especially in older adults. Because of these effects, guidelines recommend limiting long-term use.
Non-sedating antihistamines such as loratadine are often a safer option for daily allergy management, while good sleep hygiene habits can help with nighttime difficulties.
Practical Ways to Use Medications More Safely
A few small habits can support long-term health:
• Review medications each year with your doctor or pharmacist.
• Track what you take, when you take it, and why.
• Try non-medication approaches for recurring issues.
• Read labels carefully every time.
• Ask questions about safer alternatives or lower doses.
These steps allow you to stay informed and reduce unnecessary risks while still benefiting from necessary treatments.
Wrapping It Up
Thoughtful medication use is about striking a healthy balance, not giving up treatments that help you feel better. Understanding how these drugs work over time gives you the tools to talk openly with your doctor and make informed decisions. Many people are surprised to learn that small lifestyle changes—better sleep routines, improved nutrition, and regular physical activity—often reduce the need for certain medications and support a stronger sense of control over their health.
FAQ
-
Are these medications unsafe for everyone?
No. Many people use them safely for short periods or with proper medical guidance. Concerns arise mainly with frequent or prolonged use. -
How can I tell if long-term use is affecting me?
Watch for new symptoms such as unusual fatigue or digestive changes. Routine check-ups and lab tests offer valuable monitoring. -
Can I stop long-term medications on my own?
Always talk to your doctor before stopping. Some medications require gradual reduction to avoid withdrawal or rebound symptoms.
Disclaimer: This article is for informational purposes only and does not replace professional medical guidance. Always consult your healthcare provider before making any changes to medications or health routines.