1. The role of the urinary system in intimate relationships
The urinary system plays a vital role in maintaining overall health by removing liquid waste from the body and keeping chemical balance stable. Its primary organs, including the kidneys, bladder, and urethra, work continuously to filter blood and expel excess fluids. During intimate contact, however, this system can become more vulnerable to external influences, particularly in women.
In women, the urethra is relatively short and located close to the vaginal and anal areas. During sexual intercourse, bacteria naturally present on the skin or in nearby regions can be transferred toward the urethral opening. This does not indicate poor hygiene or wrongdoing; it is a biological reality linked to anatomy. Once bacteria reach the urethra, they may begin moving upward if conditions allow.
In men, the same process can occur, although it happens less frequently. The male urethra is longer, which provides additional protection against bacteria traveling toward the bladder. Even so, microorganisms can still enter the urethra during sexual activity and remain there temporarily. When urination does not follow, these bacteria are given time to settle, multiply, and potentially trigger inflammation or infection.
Understanding this connection between intimacy and urinary health helps explain why simple habits can have a meaningful impact on long-term comfort and well-being.
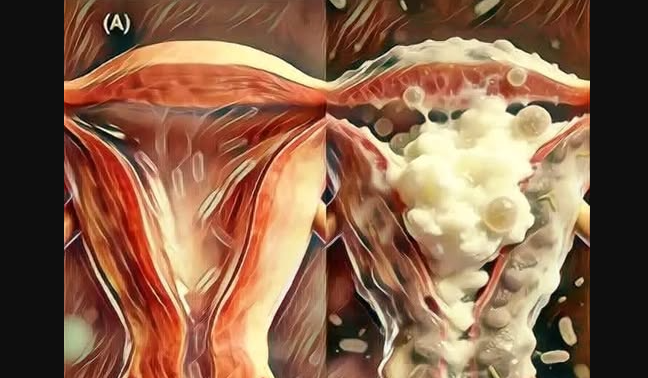
2. Postcoital cystitis: a common outcome when bacteria remain
One of the most frequently discussed consequences of not urinating after sex is postcoital cystitis. This condition refers to a urinary tract infection that develops after sexual activity, most commonly affecting women. The infection usually occurs when bacteria, often Escherichia coli, reach the bladder and cause inflammation.
Symptoms often appear several hours after intercourse rather than immediately. These may include a burning sensation during urination, a frequent and urgent need to urinate, pressure or pain in the lower abdomen, and, in some cases, fever or general discomfort. These symptoms can disrupt daily life and may require medical treatment if they persist.
Postcoital cystitis does not affect everyone, yet it is common enough that healthcare professionals regularly discuss prevention strategies. One of the simplest recommendations involves emptying the bladder after sexual intercourse. This action helps remove bacteria that may have entered the urethra before they have the opportunity to travel further into the urinary tract.
By reducing the bacterial load early, the likelihood of infection decreases significantly. This habit does not guarantee complete prevention, though it offers a practical layer of protection that supports urinary health.
3. Urination as a natural cleansing mechanism
Urinating after sex acts as a natural cleansing process for the urinary tract. As urine passes through the urethra, it helps flush out bacteria and microorganisms that may have been introduced during intimacy. This internal rinsing reduces the chance that bacteria will adhere to the urethral lining or reach the bladder.
Beyond bacterial removal, urination also relieves residual pressure in the bladder that may remain after intercourse. This can improve comfort and reduce irritation. In women, it also supports the maintenance of a balanced pH level in the intimate area, which plays an important role in preventing irritation and maintaining healthy natural flora.
This process works quietly and efficiently, relying on the body’s own systems rather than medication or intervention. While it may seem minor, the effect accumulates over time, contributing to fewer infections and greater comfort.
4. Supporting long-term urinary and intimate health
Adopting habits that support urinary health benefits people of all ages. Staying well hydrated, practicing regular hygiene, and paying attention to bodily signals all contribute to prevention. Urinating after sexual intercourse fits naturally into this broader approach.
It is also important to note that recurring symptoms, discomfort, or infections should be discussed with a healthcare professional. Individual anatomy, hormonal changes, and medical conditions can influence susceptibility to urinary issues, and personalized guidance may be necessary.
By understanding how the urinary system responds during intimacy and recognizing the value of small preventative actions, people can make informed choices that protect comfort and health. These habits encourage balance rather than reaction, supporting the body before problems arise.
In the long term, awareness and consistency create a foundation for healthier intimate experiences and reduced risk of urinary complications.